What Are the Most Effective Treatments for Anal Fissures?
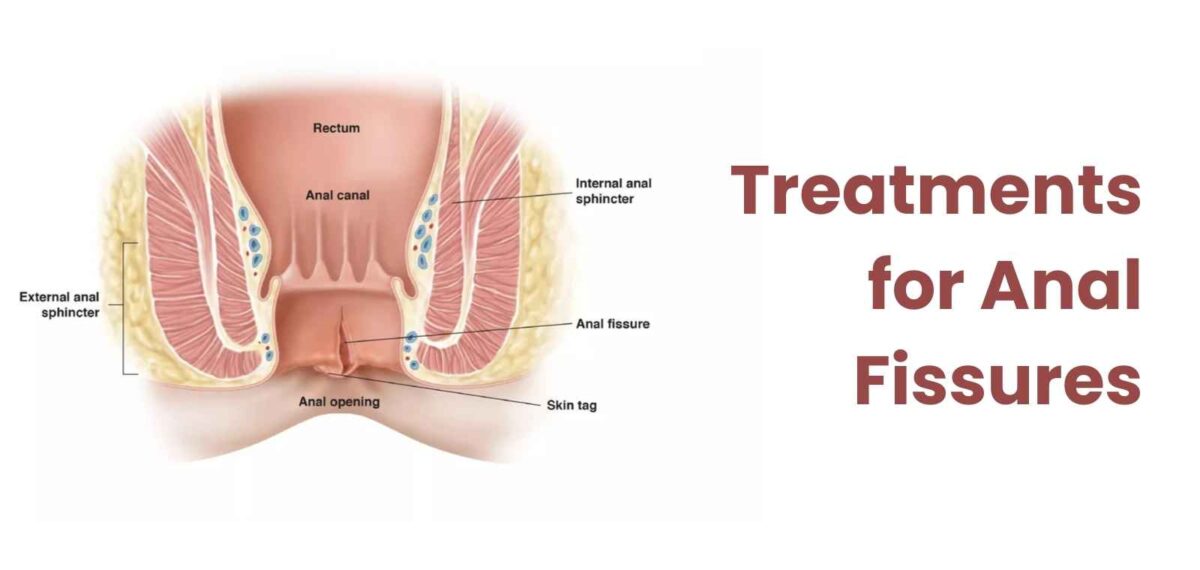
Anal fissures are small tears in the lining of the anus and are surprisingly common yet often misunderstood. According to medical research, around 11% of the population will experience an anal fissure at some point in their lives, and the condition can affect both children and adults equally. This painful condition typically causes discomfort, bleeding, and a burning sensation during bowel movements. If left untreated, fissures can become chronic, leading to more severe issues that require surgical intervention.
In this blog, we will explore the most effective treatments for anal fissures, including conservative approaches, surgical options, and recovery expectations.
What Are the Main Causes of Anal Fissures?
Before diving into treatments, it’s essential to understand the root causes of anal fissures. An anal fissure typically occurs due to trauma or injury to the anal canal. Here are some of the most common causes:
- Constipation: This is the leading cause of anal fissures. Straining during bowel movements, passing hard stools, or chronic constipation can cause a tear in the anal lining.
- Chronic Diarrhoea: Frequent bowel movements or diarrhoea can also irritate and damage the anal canal.
- Childbirth: Women may be more susceptible to anal fissures following vaginal delivery due to the physical strain and stretching of the anal area during childbirth.
- Tight Anal Sphincter Muscles: Increased tension in the anal sphincter muscle can restrict blood flow to the area, leading to tears that are difficult to heal.
- Inflammatory Bowel Diseases (IBD): Conditions like Crohn’s disease and ulcerative colitis may also increase the risk of developing fissures.
According to Dr. Mouhsen Al Hosein, “The best way to prevent fissures is to maintain healthy bowel habits through proper diet and hydration. Small lifestyle changes can significantly reduce the chances of recurrence.”
What Is the Best Treatment for Anal Fissures?
Treatment for anal fissures can vary depending on whether the condition is acute (lasting less than six weeks) or chronic (lasting more than six weeks). For most patients, the goal is to relieve pain, heal the tear, and prevent recurrence. Treatment options range from simple home remedies to more advanced medical interventions.
1. Conservative Treatment for Acute Fissures:
For acute anal fissures, non-invasive treatments are typically the first option considered. These treatments focus on relieving discomfort and promoting the healing of the tear. Some of the most effective conservative treatments include:
- Dietary Changes: One of the simplest ways to manage and prevent anal fissures is by increasing your intake of dietary fibre. Foods rich in fibre, such as fruits, vegetables, and whole grains, help soften stools and reduce the strain during bowel movements. Studies show that a diet with 20-35 grams of fibre per day can significantly lower the risk of developing fissures.
- Hydration: Drinking plenty of water (about 8-10 glasses per day) is equally essential as fibre in preventing hard stools and constipation.
- Sitz Baths: Sitting in warm water for 10-15 minutes several times a day, especially after bowel movements, can relax the anal muscles and relieve pain. This simple yet effective treatment helps increase blood flow to the affected area, speeding up the healing process.
- Topical Ointments: Medications such as nitroglycerin, diltiazem, or nifedipine are commonly prescribed to help relax the anal sphincter and promote healing. Nitroglycerin, for instance, has been shown to heal up to 70% of acute fissures within six weeks.
- Over-the-Counter Pain Relief: Anti-inflammatory drugs like ibuprofen or acetaminophen can alleviate pain, while stool softeners can reduce strain during bowel movements.
2. Surgical Options When Conservative Treatments Fail
For fissures that do not respond to conservative treatments within six weeks, surgery may be recommended. Chronic fissures often require more direct interventions, particularly if there are underlying factors like tight anal muscles or frequent spasms.
- Lateral Internal Sphincterotomy (LIS): This procedure involves making a small incision in the internal anal sphincter muscle, reducing muscle tension, and allowing the fissure to heal. Research shows that LIS has a 90-95% success rate in healing chronic fissures and relieving symptoms.
One of Dr. Mouhsen’s patients who underwent this procedure said “The surgery was life-changing. Within weeks, the pain was gone, and I could return to my normal routine. I’m so grateful for finally finding a permanent solution.”
- Botox Injections: Botox temporarily paralyzes the sphincter muscle, reducing spasms and allowing the fissure to heal. While Botox is effective, its results are typically temporary, and some patients may require repeat treatments. Success rates for Botox range between 60-80%.
- Fissurectomy: As the name suggests the fissure is surgically removed. This procedure is less common but may be necessary for large or complex fissures that do not heal with other treatments.
What Is the Cost of Anal Fissure Surgery?
The cost of anal fissure surgery in Dubai can vary depending on the hospital, the surgeon’s expertise, the type of surgery, and post-operative care. On average, the cost ranges from USD 2,700 to USD 8,200. This typically includes the surgery, hospital stay, anaesthesia, and follow-up care, but additional expenses such as pre-surgery consultations and diagnostic tests may apply. It’s essential to consult with the hospital for a detailed breakdown of costs.
What to Expect During Recovery from Anal Fissure Surgery?
Recovery from anal fissure surgery is relatively straightforward, with most patients resuming normal activities within 2 to 4 weeks. However, it’s essential to follow post-operative care guidelines to ensure proper healing and prevent recurrence.
- Pain Management: Pain is usually well-controlled with over-the-counter medications, and discomfort typically decreases within a few days.
- Diet and Hydration: Continue with a high-fibre diet and drink plenty of water to prevent constipation and ensure smooth bowel movements.
- Hygiene: Regular sitz baths and proper hygiene can help prevent infections and speed up recovery.
- Follow-Up: Post-surgery check-ups with your doctor will monitor healing progress and address any potential complications.
Conclusion
Anal fissures are a common yet manageable condition. Whether through dietary changes, topical treatments, or surgical intervention, effective treatments are available to relieve discomfort and promote healing. If you’re experiencing persistent symptoms, consult with a healthcare provider to discuss the best treatment plan tailored to your needs. With the right approach, even chronic fissures can be successfully treated, leading to long-term relief and improved quality of life.
FAQs
1. Can stress contribute to the development of anal fissures?
Yes, stress can contribute to digestive issues like constipation, increasing the risk of fissures.
2. Is it safe to exercise with an anal fissure?
Light activities like walking are generally safe, but strenuous exercises that strain the rectal area should be avoided.
3. Can dietary supplements help in fissure recovery?
Yes, fibre supplements can soften stools and ease bowel movements, promoting healing.
4. Can anal fissures be mistaken for haemorrhoids?
Yes, both cause pain and bleeding, but they are different conditions that require different treatments.
5. Can anal fissures lead to cancer?
No, fissures themselves do not lead to cancer, though a doctor should evaluate chronic issues.
Explore more blogs: What Are the Common Causes of Anal Fissures?

